Scarring is one of the most common concerns for patients considering a breast lift (mastopexy). While incisions are a necessary part of the procedure, their size, location, and long-term visibility can vary widely. This article covers what breast lift scars typically look like, how they heal, and the steps that can be taken to reduce their appearance over time. It also explains the different surgical techniques and aftercare practices that influence scarring, helping patients make informed decisions before surgery.
Types of Breast Lift Techniques and Associated Scars
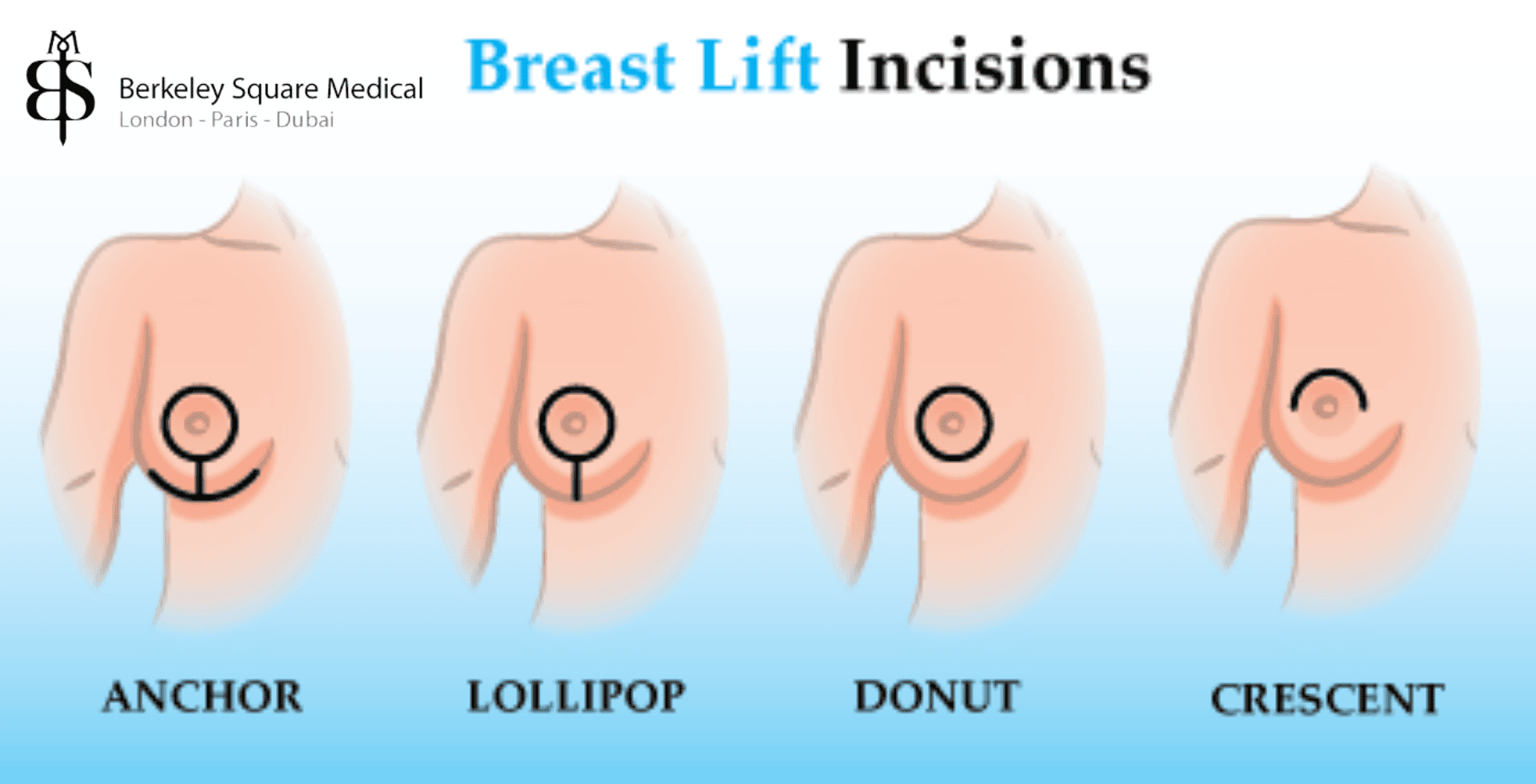
Several techniques can be used for a breast lift, each resulting in different types and extents of scarring. Here is an overview of the most common techniques and the associated scars:
Donut Technique (Periareolar)
The Donut Technique involves a circular incision around the areola. This method is ideal for patients needing minimal lift. The scar is typically well-hidden along the natural border of the areola, making it less noticeable due to the colour difference between the areola and surrounding skin.
Crescent Technique
The Crescent Technique involves a small, crescent-shaped incision along the upper half of the areola. This technique is suitable for minor lifts and can be particularly effective when combined with other breast procedures. The scar is discreetly positioned around the upper edge of the areola.
Lollipop Technique (Vertical)
The Lollipop Technique, or vertical lift, includes an incision around the areola and a vertical incision from the bottom of the areola to the breast crease. This method provides more significant lift and reshaping. The resulting scars are more visible than those from the Donut or Crescent techniques but can still be well-concealed with proper care.
Anchor Technique (Inverted-T)
The Anchor Technique, also known as the Inverted-T lift, involves three incisions: around the areola, vertically from the areola to the breast crease, and horizontally along the breast crease. This method is used for the most substantial lifts and reshaping. While it results in more extensive scarring, these scars can be strategically placed to be less noticeable and are often hidden in the natural breast fold.
Horizontal Technique
Though less commonly used, the horizontal lift involves an incision along the breast crease without any vertical or areolar incisions. It’s typically reserved for patients requiring minimal correction to the lower part of the breast. Scarring is generally limited to the inframammary fold.
What Do Breast Lift Scars Look Like Over Time?
Scars from a breast lift go through several stages of healing. Initially, they may appear red, raised, and slightly swollen. Over time, they generally flatten and fade in colour.
- 0–3 months: Scars are usually pink or red and may be raised. This is a normal inflammatory response as your body starts the healing process. The area may feel slightly firm or itchy, but discomfort typically lessens within a few weeks.
- 3–6 months: The colour begins to fade, and the scars flatten out. Collagen remodelling is underway during this stage, which leads to softer and less prominent scars. At this point, you may start using treatments like silicone gel if approved by your surgeon.
- 6–12 months: Scars continue to lighten, becoming closer to your natural skin tone. Most patients report a noticeable improvement in texture and colour by this stage, though some redness or slight elevation may persist.
- 12+ months: For many patients, scars become faint and less noticeable. However, this varies based on individual healing and scar care. Some may have residual pigmentation or mild raised areas, but these often continue to improve well into the second year post-op.
Factors such as sun exposure, proper wound care, and skin type significantly influence how quickly scars fade. Some patients may benefit from scar treatments during this period to speed up the process or improve outcomes.
Types of Scars That Can Form
Not all scars heal the same way. Depending on your skin type, genetics, and healing process, you may experience:
- Hypertrophic Scars: Raised, red scars that stay within the incision line.
- Keloid Scars: Raised, thick scars that grow beyond the incision. More common in individuals with darker skin tones.
- Atrophic Scars: Sunken or pitted scars, less common after mastopexy but possible.
- Pigmented Scars: Some patients may develop darker or lighter areas of pigmentation depending on skin tone and healing.
Your surgeon can advise on strategies to minimise or treat these scar types. Early intervention is key to managing hypertrophic and keloid scarring.
Factors Influencing Scarring
The extent and visibility of scarring after a breast lift are influenced by several factors, each contributing to the overall healing process and final appearance of the scars:
- Amount of Lift Required: Larger lifts generally require more incisions, resulting in more noticeable scars.
- Skin Type and Healing Process: Genetics, skin elasticity, and tone influence how your scars heal. Some may develop keloids or dark pigmentation.
- Surgeon’s Skill and Technique: An experienced surgeon will use precise incision placement and advanced suturing techniques to promote better healing.
- Use of Implants with Breast Lift: Augmentation mastopexy can involve different incision patterns, possibly leading to additional or longer scars.
- Lifestyle Factors: Smoking, poor nutrition, and excessive physical activity during recovery can negatively impact wound healing and scar formation.
- Post-Operative Compliance: Following post-operative care instructions diligently is essential for optimal scar formation.
Watch Video
Pre-Operative and Post-Operative Care
Proper care before and after the surgery is essential for optimal scar healing. Here are key considerations and steps to ensure the best outcomes:
Pre-Operative Considerations
- Choosing an Experienced Surgeon: Selecting a skilled and experienced surgeon is the first step in minimising scars. Look for a board-certified professional with a strong track record in breast lifts. Ask to see before-and-after photos of previous patients to assess their typical scar outcomes.
- Discussing Expectations and Scar Management: A thorough discussion with the surgeon about the expected results and scarring can help set realistic expectations. Be sure to ask about incision placement and any strategies they use to reduce scarring, such as layered closure techniques or post-op scar therapy.
- Preparing the Skin: Some surgeons may recommend pre-operative skincare routines to improve skin condition and elasticity. This could include moisturisers, gentle exfoliants, or prescription creams if you have conditions that might impair healing. Healthy, hydrated skin is more resilient and tends to heal more effectively.
Post-Operative Care for Optimal Scar Healing
- Follow Post-Op Instructions: Proper wound care, wearing supportive garments, and attending follow-ups are essential. Your surgeon will provide a detailed recovery plan tailored to your procedure, and adhering to it closely helps minimise complications and support healthy scar formation.
- Avoid Certain Activities: Avoid heavy lifting, smoking, and sun exposure during the healing period. Physical strain can stretch the incision site, while smoking reduces blood flow, impeding the body’s ability to repair tissue. Direct sunlight on fresh scars can cause dark pigmentation and delay fading.
- Use Silicone Gels and Sheets: These products can help flatten and lighten scars by hydrating the area and promoting collagen remodeling. They are typically applied once the incisions have closed and can be used daily for several months. Studies have shown that silicone products are among the most effective non-invasive scar treatments.
- Maintain Proper Hygiene: Keeping incisions clean and dry reduces the risk of infection, which can worsen scarring. Use only approved cleansers and pat the area dry with a clean towel. Avoid submerging the area in water until your surgeon confirms it’s safe.
- Sleep in the Right Position: Sleeping on your back with your upper body elevated can reduce pressure on the chest and aid healing. Elevation also helps minimise swelling and fluid retention, which can improve comfort and prevent stress on incisions.
- Nutrition and Hydration: A diet rich in vitamins A and C, zinc, and protein supports the body’s healing process. Hydration is also key, as it supports tissue regeneration and reduces the risk of dry or irritated skin at the incision site.
Treatment Options for Scar Reduction
If scars are more visible than desired, several treatment options may help:
- Laser Therapy: Helps reduce redness and smooth scar texture. It can also stimulate collagen production, which can help blend the scar with surrounding skin. Fractional lasers or pulsed dye lasers are commonly used for surgical scars.
- Steroid Injections: Used to treat hypertrophic or keloid scars. These injections reduce inflammation and slow down excessive collagen production. They may be administered in a series of sessions spaced several weeks apart.
- Microneedling: Stimulates collagen production to improve scar appearance. This involves tiny needles creating micro-injuries in the scar tissue to promote regeneration. It’s often combined with serums or platelet-rich plasma (PRP) for enhanced results.
- Scar Revision Surgery: A surgical option to remove or improve unsightly scars. The new incision is often placed in a less visible location or closed using advanced techniques to encourage better healing. This is typically reserved for scars that are unusually wide, thick, or misaligned.
- Chemical Peels or Dermabrasion: Can improve skin texture and tone. These resurfacing treatments work by removing the top layers of skin to reveal newer, smoother skin underneath. They are most effective for superficial scar irregularities or pigmentation.
- Pressure Therapy: Compression garments or silicone tape may help flatten raised scars. Applying pressure to the area can reduce blood flow to the scar tissue and slow its growth, especially when used early in the healing process.
- Radiotherapy: Rarely used, but may be considered in severe keloid cases. It is generally a last-resort treatment due to potential risks, and only considered when other treatments have failed.
Always consult your surgeon before pursuing additional treatments. Many of these interventions work best when started within a few months post-op.
Frequently Asked Questions
Will my breast lift scars go away completely?
Scars will fade significantly over time, often becoming barely visible, but they will not disappear completely.
Can I have a scarless breast lift?
No surgical breast lift is completely scarless, but techniques like the Crescent or Donut lift leave minimal, discreet scarring. Non-surgical treatments, like skin tightening devices, do not produce lift results comparable to surgery.
How long do scars take to heal?
Most scars improve dramatically within 6–12 months, though healing varies by individual. Full scar maturation may take up to 18 months.
What if my scars are raised or itchy?
This may indicate a hypertrophic or keloid scar. Speak to your surgeon about treatment options like steroid injections, pressure therapy, or silicone sheets.
How can I prevent bad scarring?
Follow all post-op instructions, avoid sun exposure, don’t smoke, maintain proper nutrition, and consider using recommended scar treatments.
Does breast skin tone affect scar appearance?
Yes. Darker skin tones may be more prone to hyperpigmentation or keloid scars. Your surgeon can tailor aftercare accordingly.
Can I cover breast lift scars with makeup or tattooing?
Camouflage makeup or medical tattooing can be used once the scar is fully healed. Consult a dermatologist or medical tattoo specialist.
Considering a Breast Lift?
It’s completely natural to feel concerned about breast lift scars. The good news is that with a skilled surgeon, proper aftercare, and some patience, most patients find that their scars fade significantly and are well-hidden by natural breast contours. Understanding the healing timeline and proactively managing scar care can make a meaningful difference in long-term outcomes.
If you have concerns about scarring or want to understand more about the options available to you, a consultation with an experienced surgeon is the best next step.
For more information about Breast Lift Surgery , visit our Breast Lift Page or contact us at info@berkeleysquaremedical.com to arrange a consultation with our team of Consultant Breast Lift Surgeons.
Sanjay is a Senior Clinical Member at Berkeley Square Medical carrying over a decade of experience. He has assisted over 1500 surgeries carried out at the hospital supporting patients both pre and post-surgery throughout their treatment journeys. This article was written with the contribution of
Dr Taimur Shoaib, our Consultant Plastic Surgeon.
Latest posts by Sanjay Rai
(see all)
